Sesamoiditis and Its Role in Ball of Foot Pain
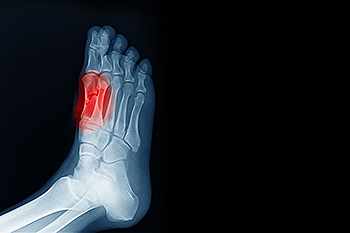
Sesamoiditis is a condition that involves inflammation of the sesamoid bones, which are two small bones located beneath the big toe joint. These bones help with the pressure and movement of the toe during walking and running. Sesamoiditis is a common cause of metatarsalgia, a condition characterized by pain and inflammation in the ball of the foot. The most common cause of sesamoiditis is repetitive pressure or trauma, often resulting from activities like running or wearing ill-fitting shoes. Symptoms of sesamoiditis include pain under the big toe, swelling, and tenderness, particularly when walking, running, or pressing on the area. The pain may worsen with activities that put extra pressure on the feet. To diagnose sesamoiditis, a podiatrist will typically conduct a physical exam and may order imaging tests like X-rays or MRI scans to confirm the diagnosis and rule out other conditions. If you have pain in this area of your foot, it is suggested that you schedule an appointment with a podiatrist who can accurately diagnose and treat sesamoiditis.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact Dr. Eugenio Rivera of Calo Foot & Ankle Specialists. Our doctor will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact our office located in Bellaire, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sesamoiditis
Sesamoiditis is a condition in which the sesamoid bones in the forefoot become inflamed from physical activity. Sesamoid bones are bones that are not connected to other bones but are located in tendons or muscle. Two of these sesamoid bones are very small and located on the underside of the foot near the big toe. Athletes such as runners, baseball and football players, and dancers are likely to experience sesamoiditis. Those with high arched feet, flat feet, or runners who run on the ball of their foot are also prone to suffer from sesamoiditis.
Symptoms include pain or throbbing on the ball of the foot near the big toe. The pain generally starts with a mild throbbing but gradually builds up to shooting pain. Bruising, swelling, and redness are possible, but in most cases, these symptoms are not present. However, moving the big toe can result in pain and difficulty.
To conduct a diagnosis, the podiatrist will examine the ball of the foot and big toe. They will look for any outliers and check the movement of the toe. X-rays will be taken to rule out any other conditions and ensure that it is sesamoiditis.
Treatment for sesamoiditis is generally mild and includes rest, anti-inflammatory and pain medication, and ice treatments to deal with the swelling and pain. Orthotics may be needed with people who have flat or high arched feet to relieve pressure off the bones. In some cases the toe will be taped and immobilized to allow healing. The podiatrist may also decide to use a steroid injection to help with swelling as well. If you have sesamoiditis, you shouldn’t engage in any intensive activity, as it may inflame the area and worsen your pain. If the sesamoid bone has fractured, surgery may be required to remove the sesamoid bone.
If you are suffering from sesamoiditis or are experiencing symptoms similar to sesamoiditis, you should stop all physical activity that puts strain on the area. Furthermore you should see a podiatrist for a diagnosis to see if you have sesamoiditis.
What Is a Shoe Bite?

A shoe bite refers to a painful irritation or blister that forms on the skin due to friction between the feet and ill-fitting shoes. These blisters typically appear on areas like the heels, toes, or sides of the feet. The primary cause of shoe bites is wearing shoes that are too tight, too loose, or made from stiff materials that rub against the skin. This constant friction leads to skin damage, causing redness, swelling, and eventually blisters. To prevent shoe bites, it is essential to choose shoes that fit well and provide adequate support. Using blister pads or cushioned insoles can also help reduce friction. Additionally, breaking in new shoes gradually and wearing socks made from breathable materials can protect the skin from excessive rubbing. Untreated blisters may become infected and become quite painful. If you have developed a foot blister, it is suggested that you consult a podiatrist who can offer additional prevention tips, and provide effective relief methods.
Blisters may appear as a single bubble or in a cluster. They can cause a lot of pain and may be filled with pus, blood, or watery serum. If your feet are hurting, contact Dr. Eugenio Rivera of Calo Foot & Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters are often the result of friction. This happens due to the constant rubbing from shoes, which can lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
Symptoms
(Blister symptoms may vary depending on what is causing them)
- Bubble of skin filled with fluid
- Redness
- Moderate to severe pain
- Itching
Prevention & Treatment
In order to prevent blisters, you should be sure to wear comfortable shoes with socks that cushion your feet and absorb sweat. Breaking a blister open may increase your chances of developing an infection. However, if your blister breaks, you should wash the area with soap and water immediately and then apply a bandage to the affected area. If your blisters cause severe pain it is important that you call your podiatrist right away.
If you have any questions, please feel free to contact our office located in Bellaire, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters
Blisters are pockets of fluid that occur under the top layer of your skin. These fluid pockets are usually filled with pus, blood, or serum. Blisters may itch or hurt and can appear as a single bubble or in clusters.
The most common types of blisters are friction blisters. This type of blister may be caused by wearing shoes that are too tight. Friction blisters can also occur on the hands. A change in temperature may also cause blisters on the feet. In the freezing air, frostbite on your toes can lead to blisters, as well as sunburn from hot weather.
The best way to treat a blister is to keep it clean and dry. Most blisters will get better on their own. Once the skin absorbs the fluid within the blister, it will flatten and eventually peel off. You should avoid popping your blister unless you podiatrist does it for you. Additional treatment options include applying an ice pack to the blister or using over-the-counter blister bandages to cover the affected area.
If your blister becomes discolored, inflamed, or worsens it is advised that you speak to your podiatrist. Blisters that are yellow, green, or purple may be infected and require immediate medical attention. Blisters that are abnormally colored may be a sign of a more serious underlying health condition such as herpes.
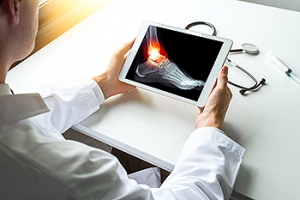
Causes and Recovery Time for a Broken Ankle
A broken ankle typically occurs due to trauma or impact, such as a fall, sports injury, or car accident. It can also happen from twisting or rolling the ankle in an awkward position. Common symptoms include pain, swelling, bruising, and difficulty walking or bearing weight on the affected foot. In some cases, the bone may protrude through the skin, indicating a more severe fracture. The severity of the injury can vary, with some fractures requiring surgery and others treated with a cast or brace. Recovery time for a broken ankle depends on the type and severity of the fracture. Generally, it can take six to eight weeks for the bone to heal, but full recovery, including regaining strength and mobility, may take several months. If you have broken your ankle, it is suggested that you promptly visit a podiatrist who can offer effective treatment solutions.
Broken ankles need immediate treatment. If you are seeking treatment, contact Dr. Eugenio Rivera from Calo Foot & Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact our office located in Bellaire, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Broken Ankle Causes, Differences, Symptoms and Treatments
The ankle is a hinged synovial joint made up of three bones: the tibia (shin bone), the fibula (outer ankle bone), and the talus (between the heel and leg). These three bones are bound, supported, and stabilized by strong, fibrous bands of tissue called ligaments.
A break in an ankle bone can be either traumatic or stress related. This injury may be referred to as a break or fracture. A traumatic fracture can result from tripping, twisting or rolling the ankle, falling, or by blunt impact to the ankle. These traumatic ankle breaks usually occur during sporting activities or accidents. Stress fractures, however, occur over time and are the result of repetitive stress to the ankle. These fractures sometimes occur when a new activity that engages the ankle is introduced, or when the level of activity is abruptly increased or intensified.
There are various symptoms that accompany an ankle break. The most significant symptoms are pain and swelling that occurs in the ankle and sometimes spreads up from the foot to below the knee. Bruising or discoloration may develop eventually. It will be difficult or even impossible to put weight on the affected foot, and in severe cases there may be a visible deformity or even exposed bone.
It is very important to seek immediate treatment when an ankle break occurs or is suspected to have occurred, in order to allow the bone to properly heal and to avoid future complications such as stiff joints, limited range of motion, and osteoarthritis.
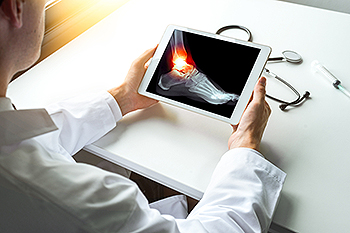
To diagnose a broken ankle, your podiatrist will first ask you to explain how the injury occurred and what your symptoms are. They will perform a thorough examination, checking for damage to nerves, blood vessels, and other structures around the injury site. They will also test your range of motion. An X-ray will need to be reviewed and, in some cases, an MRI or CT scan may be necessary.
Proper treatment of a broken ankle will depend on where and how severe the break is, how stable the ankle is, and whether the bone is displaced (misaligned or separated) or non-displaced (broken yet still aligned properly).
Mild fractures (where the bone is non-displaced) may be treated by resting, icing, and elevating the ankle at first, followed by immobilization with a cast or walking boot. Pain and inflammation may be treated with acetaminophen. More severe or complicated fractures where bones or joints are displaced may require surgery.
Recovery time will also vary, and it may take 4-6 weeks or longer for a broken ankle to heal. Your podiatrist will most likely order progressive X-rays or stress tests to be taken in order to monitor the healing process.
Managing Plantar Warts

Plantar warts are small, rough growths that appear on the soles of the feet, caused by the human papillomavirus, known as HPV. These warts are contagious and can spread through direct contact or by walking barefoot in public places like swimming pools and locker rooms. People with weakened immune systems, such as those with diabetes, HIV, or undergoing chemotherapy, are more likely to develop plantar warts. The virus thrives in warm, moist environments, making feet particularly vulnerable. Plantar warts can be painful, especially when pressure is applied while walking, and may appear with tiny black dots at their center, which are blood vessels. While treatments like salicylic acid can help, they often take time and may not work for deeper or larger warts. A podiatrist can offer a proper diagnosis and suggest effective treatment for plantar warts. Treatment options include cryotherapy, laser therapy, or minor surgical removal for faster, more lasting results. If you have a plantar warts, it is suggested that you schedule an appointment with a podiatrist.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dr. Eugenio Rivera from Calo Foot & Ankle Specialists. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Bellaire, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Are Plantar Warts?
Plantar warts are described as small growths that appear on the heels or other areas of the feet that bear a large amount of weight. The pressure in these areas causes plantar warts to hide behind thick layers of skin called calluses. In most cases, plantar warts are not a serious health issue, and they usually go away without treatment. However, it is still important be mindful of them.
Plantar warts are caused by infections with human papillomavirus (HPV) in the outer layer of skin on the soles of the feet. The plantar warts then develop when the virus enters the body through weak spots at the bottom of the feet, such as tiny cuts and breaks. Plantar warts are not guaranteed for all who encounter the virus. Everyone responds differently to the affects of HPV.
Plantar warts are most common in the following groups: children and teenagers, people with weakened immune systems, people with history of plantar warts, and people who walk barefoot. Exposure to HPV is common in environments such as locker rooms or pool areas.
One of early signs to look out for is a callus, since many plantar warts hide behind them. You can also locate these warts by looking for small, fleshy, rough, grainy growths near the base of the toes and the heel. Early signs of plantar warts are shown by black pinpoints, which are small, clotted blood vessels. Lesions that interrupt normal lines and ridges in the skin of your foot may also be a sign of plantar warts. Any feeling of pain while walking or standing can also be a symptom of plantar warts.
Although most cases are not serious, some conditions may require a visit to your podiatrist. If you are uncertain that your lesion is a wart, if you have diabetes, or if you are experiencing bleeding, you may need to see a seek professional treatment. Your doctor may offer treatments such as prescribing stronger peeling medicine or using cryotherapy by applying liquid nitrogen to the wart. More serious cases may require minor surgery or laser treatment.
There are simple solutions available to help prevent plantar warts. One common task is to avoid walking barefoot in swimming pool areas and locker rooms, as this is where HPV is commonly present. Keeping your feet clean and dry, while changing shoes and socks daily can also help prevent future plantar warts. If you know someone who has plantar warts, it is important to avoid direct contact with their warts. You should also refrain from picking or scratching your wart if you happen to develop one.
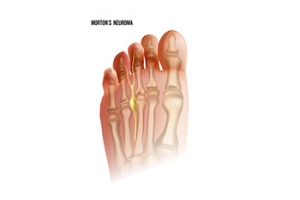
Symptoms and Causes of Morton’s Neuroma
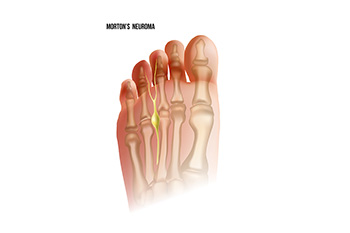
Morton's neuroma is a painful condition that affects the ball of the foot, typically between the 3rd and 4th toes. It occurs when the tissue surrounding a nerve becomes thickened, causing irritation or compression. The exact cause of Morton's neuroma is not always clear, but factors like wearing tight or ill-fitting shoes, particularly high heels, can contribute by putting pressure on the ball of the foot. Other causes include repetitive stress or activities that involve high-impact movements, like running or jumping. Symptoms of Morton's neuroma include sharp, burning pain in the ball of the foot, tingling or numbness in the toes, and a feeling of something being stuck or bunched up in the shoe. These symptoms are often aggravated by walking or standing for long periods. If you have any of these symptoms, it is suggested that you contact a podiatrist who can successfully treat Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Eugenio Rivera of Calo Foot & Ankle Specialists. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Bellaire, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.